19 Jun Avoiding Transmission of Community Acquired Infections
“Community-acquired infections” (CAI’s) occur in all parts of the world and can be caused by several types of pathogens. Many factors, such as climate change, the aging population and the ease of global travel have contributed to the widespread exposure of the global population to diseases caused by CAI’s. Pathogens spread these infectious diseases through the air, food, insects, and even sexual activity. When people with a CAI enter a health care facility, their condition threatens everyone within the building. For healthcare professionals tasked with preventing the transmission of any disease, it is critically important to identify and contain the community-acquired condition before it can spread to an already vulnerable population.
Many Pathogens = Many Infections
Many pathogens are responsible for causing CAI’s. Viruses, protozoa, bacteria, and fungi exist in all regions. Unclean water is a frequent source of CAI’s and microbes ingested when drinking contaminated water or eating food washed in contaminated water can cause debilitating diarrhea, blindness, and death. Insects carry CAI’s, too. Mosquitos spread infectious diseases like malaria, Yellow fever, and the recently encountered Zika virus. Ticks, sandflies, fleas and triatomine bugs can also transmit disease by picking up the disease from an infected host and transmitting by biting and injecting the virus into a non-infected host. Among humans, the transmission of CAI’s frequently occurs through contact with infected tissue or blood. Unprotected sexual contact causes the AIDS virus and some of the strains of Hepatitis.
Common Symptoms
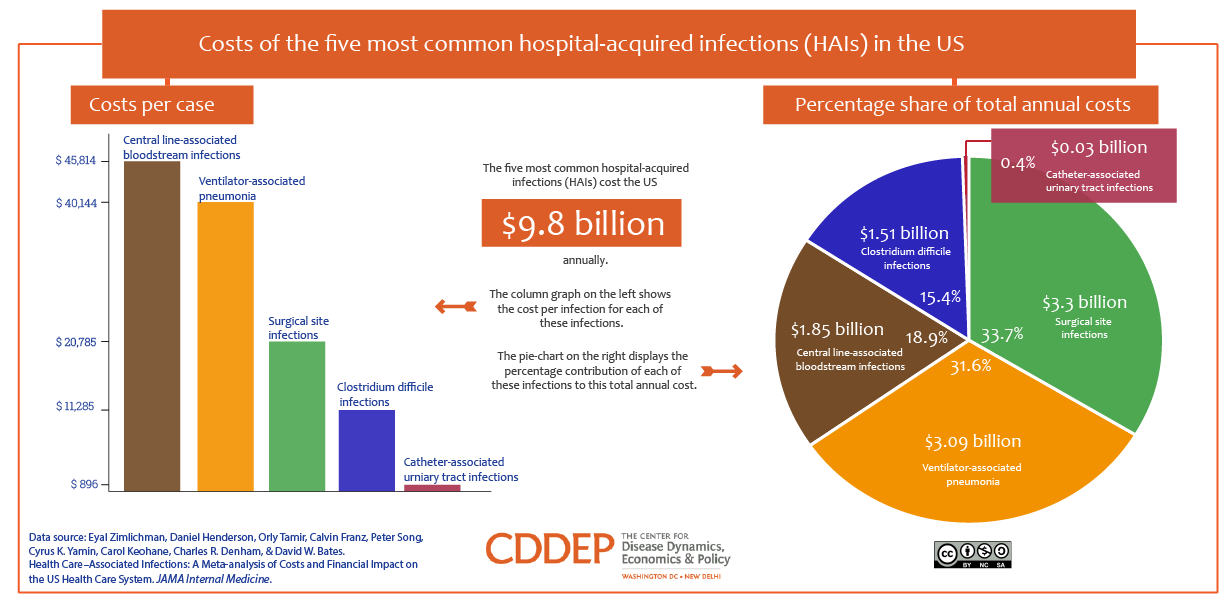
CAI’s can affect any aspect of the body. Lung and respiratory infections such as Pneumonia are relatively common in people with compromised immune systems who come into contact with a CAI pathogen. Urinary tract, skin, and digestive tract infections are also commonly caused by pathogens picked up in the environment or through contact with an infected person.
Drug-resistant CAI’s
For decades, the medical community treated every type of CAI with antibiotics, regardless of whether its cause was a bacteria or a virus. That practice, unfortunately, has resulted in the development over time of drug-resistant CAI’s. The emergence of these drug-resistant CAI’s now makes it much more challenging to slow or stop the transmission or treatment of the disease because there are no longer effective medicines available for that purpose.
Preventing Transmission of a CAI
Because medicines no longer work with some of these CAI’s, preventing transmission is now considered the best course of action when dealing with a CAI:
- Keep sick people away from healthy people. Recent c reports demonstrate that up to 90 percent of workers who lose workdays due to infectious diseases such as the flu contracted that disease through contact with an infected co-worker.
- Screen for fever in workers at risk of infection, such as those that work in hospitals, clinics or other locations with sick people gather. Studies have shown that this inexpensive procedure catches not just symptomatic individuals, but also those who are not yet displaying symptoms.
- Use tools to prevent exposure. Face masks and gloves present barriers to germs and can prevent wearers from contracting the disease of the patient with whom they are working.
- Train all workers on CAI-control best practices, including the proper sterilization techniques for locations and equipment, effective sanitation practices, and consistent use of preventative measures such as masks, gowns, and gloves.
At Infection Control Results, we train health care personnel on appropriate infection assessments and preventions.
